Connect With Us

Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
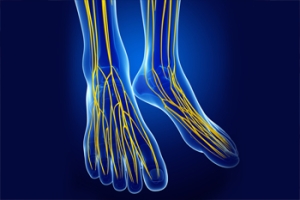
Nerve Compression in the Ankle May Cause Pain, Burning, and Numbness
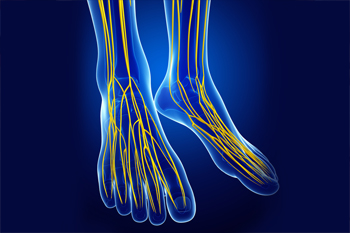
There is a narrow passageway called the tarsal tunnel, which is located on the inside of the ankle. The tibial nerve, starting at the back of the leg, runs down through the tarsal tunnel, along with veins, arteries, and tendons. Because so many structures pass through the tarsal tunnel, the interior space is very confined. This space becomes even more constricted if an ankle injury occurs that causes inflammation or a swollen vein or tendon, or if a cyst develops within the tunnel. This can cause the tibial tendon to become squeezed, or compressed, and result in pain, burning, tingling, or numbness along the nerve’s path. This condition is known as tarsal tunnel syndrome. Flat feet, and inflammation due to arthritis and diabetes may also contribute to this condition developing. It is important to have tarsal tunnel syndrome diagnosed and treated as early as possible, not only to relieve pain and inflammation, but to avoid permanent nerve damage. A podiatrist can assess your condition and devise an appropriate treatment plan to get you on the road to recovery as soon as possible.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Fox Valley Foot and Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Easy to Spot a Bunion

A bunion is easy to notice. It is classified as a deformity and is a bony protrusion on the side of the big toe. It can develop as a result of genetic factors or from wearing shoes that are too tight in the toe area. Research has shown it affects approximately 35% of people who are over 65 years old and may affect their quality of life if not promptly treated. The medical term for a bunion is called hallux valgus and happens when the first long bone of the foot meets the first bone of the toe. When this moves out of alignment, a bunion has formed. It often develops slowly and if it becomes severe it may shift the other toes toward each other. Flexibility and range of motion may negatively affect the foot, and the skin may become irritated. Some patients experience foot injuries, and this may lead to the development of a bunion. Additionally, existing medical conditions including flat feet and rheumatoid arthritis may increase the risk of getting a bunion. If you have noticed a bunion on your foot, it is strongly suggested that you are under the care of a podiatrist who can determine what the best course of treatment is for you, which may include surgery for permanent removal.
If you are suffering from bunion pain, contact one of our podiatrists of Fox Valley Foot and Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Stretches That May Help the Pain of Morton’s Neuroma
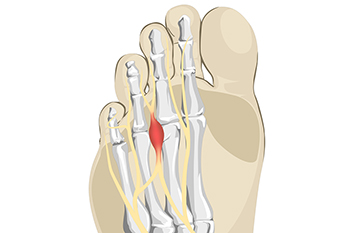
The foot condition that is known as Morton’s neuroma affects the nerve between the third and fourth toes. In severe cases, it is quite painful. This can possibly be treated without surgery in the beginning stages. It happens as a result of wearing shoes that do not have adequate room for the toes to move freely in. High heels fit into this category, and it is suggested to refrain from frequently wearing them. The nerve can gradually become compressed, and it will feel like there is a pebble in the sock or shoe. Additional symptoms can consist of burning pain and numbness in the toes. The pain may radiate to the ball of the foot, and it can be difficult to complete daily activities. A qualified doctor can perform a diagnosis by having an X-ray taken, and this can be helpful in ruling out a stress fracture. An MRI or ultrasound can also be performed, and these can eliminate conditions that may include bursitis and Freiberg’s disease. Some patients find it helpful to stretch the Achilles tendon and plantar fascia, which are located on the bottom of the foot. This may help to reduce a portion of the pain. If you have Morton’s neuroma, it is suggested that you meet with a podiatrist who can recommend the best treatment for you.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Fox Valley Foot and Ankle Specialists. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
The Danger of Ignoring Toenail Fungus

Toenail fungus, or onychomycosis, can be an unsightly condition to have. It usually appears as a white or yellow spot under the tip of the toenail. This infection often comes from walking barefoot in a public bathroom, locker room, or swimming pool area. It is important to treat this condition immediately to prevent it from worsening, spreading, or causing more serious complications. The fungi that cause this infection are contagious and can spread to other parts of the body, even the blood. Most often, they spread to other nails on the feet or hands. Antifungal medicine is usually used to combat the problem. Ways to prevent toenail fungus include using antifungal powder on the feet each day, not sharing shoes or socks, washing and drying feet regularly, wearing breathable shoes, and not walking barefoot. If you suspect you have toenail fungus, contact a podiatrist as soon as possible for proper diagnosis and treatment.
For more information about treatment, contact one of our podiatrists of Fox Valley Foot and Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.